
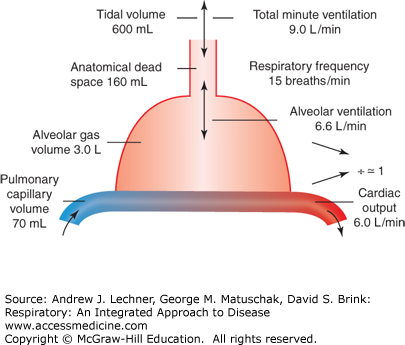
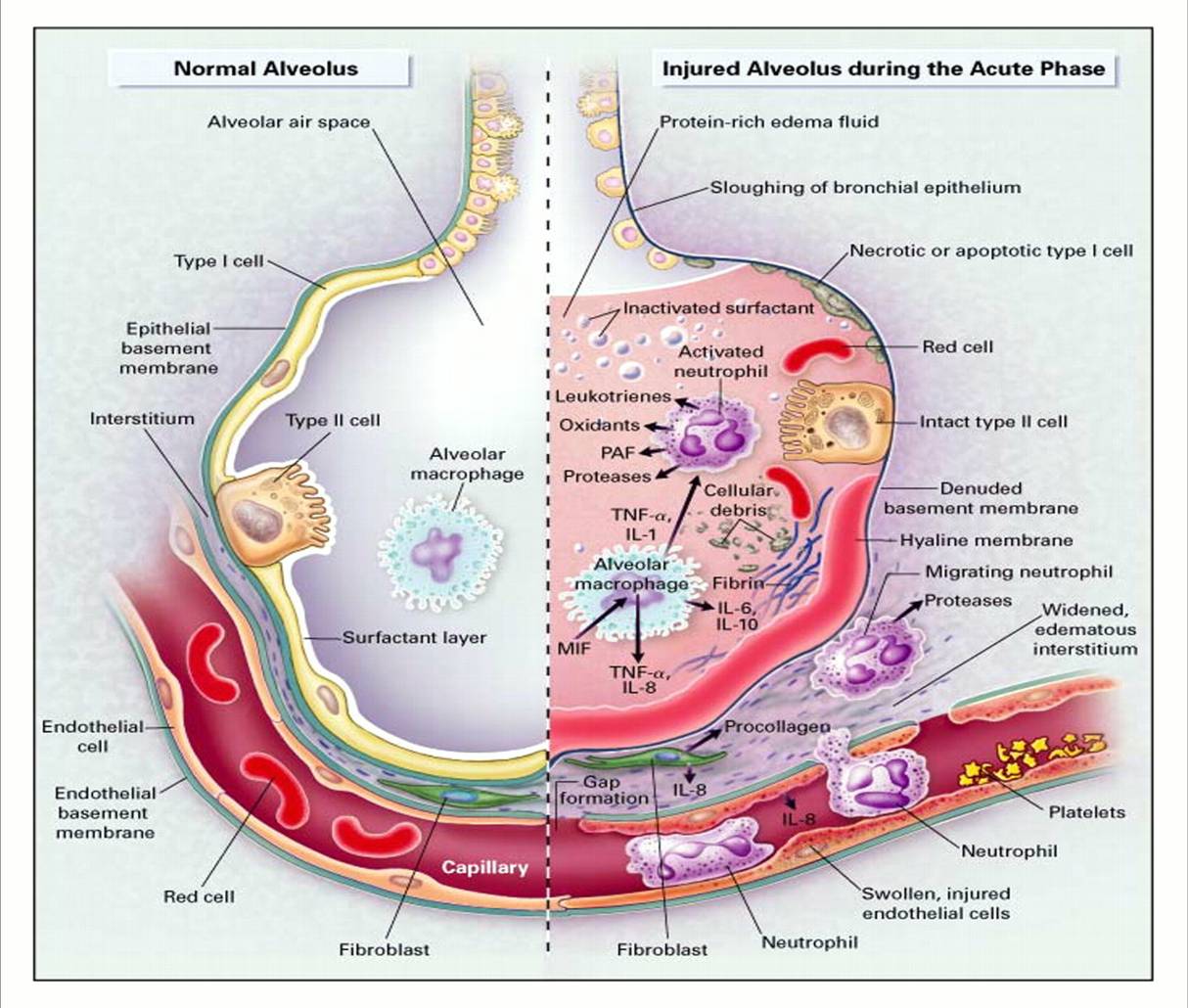
Waveform capnography should be monitored in all intubated patients and displayed on the monitor (as above).etCO2 is a measurement of the partial pressure of CO2 in gas expired at the end of exhalation (when exhaled gas will most closely resemble the alveolar CO2 concentration).Understanding how to interpret etCO2 waveforms.Understanding changes in etCO2 within the context of other data (especially trends in minute ventilation).Paying attention to etCO2 values (e.g., noting them daily in reviews of the patient, along with other vital signs).Within the next decade, continuous waveform capnography will likely become a universal standard of care across all well-resourced intensive care units.Īs the use of waveform capnography expands, we need to be thoughtful about integrating this into our practice. Capnography is increasingly recommended both to confirm endotracheal tube insertion and to subsequently monitor the patency and effectiveness of ventilation throughout the duration of intubation. Capnography was pioneered in the operating room, but the safety implications for all critically ill patients are clear (the standard of safety monitoring in the ICU shouldn't be lower than in the operating room). Failure to use waveform capnography contributed to >70% of ICU-related airway deaths in the NAP4 audit. Waveform capnography is emerging as a standard monitoring tool to improve safety among intubated patients. Ventilation may exceed perfusion in parts of the lung resulting in increased physiological dead air space.Introduction – an emerging standard of care Air may reach the periphery of the lungs but fail to make contact with the capillary blood. The alveoli become permanently damaged (see video above).This is why breathlessness and fatigue are common symptoms of COPD. This extra effort can make the patient feel very tired. However, this does not mean that your oxygen levels are low because the breathing muscles around the chest are working harder to compensate. The respiratory muscles then have to work harder to get air in and out of your lungs.As the lungs become hyper-inflated they elongate and flatten, which means the diaphragm does not work as well as it should. As a result, air gets trapped in the lungs and the lungs get bigger (hyper-inflated). These changes cause the air sacs (alveoli) to close before you have fully exhaled. In emphysema, exposure to an irritant over many years causes an inflammation in the lungs which causes the following changes: Please note there is no audio for this animation


 0 kommentar(er)
0 kommentar(er)
